Cultivated Autologous Oral Mucosal Epithelial Transplantation
Table of Contents
- ・ What is the regenerative medicine for the cornea?
- ・ Target disease
- ・ When is the treatment performed?
- ・ Regenerative medicine for the cornea provided by Kyoto Prefectural University of Medicine
- ・ Major test items and monitoring parameters and the schedule of the tests/monitoring at Kyoto Prefectural University of Medicine
- ・ To patients who hope to receive corneal regenerative treatment
What is the regenerative medicine for the cornea?
We are leading our daily lives with most of the information from the outside world obtained through sight (the eye). The cornea (on the iris ) is an important transparent part that controls vision. If the cornea is damaged by various causes, it will lose its transparency and have significant visual impairment. Corneal transplantation with a cornea from an eye donated to an eye bank had been performed to treat such clouded corneas in the past. Corneal transplantation has often been successful and has recovered eyesight in many patients. However, because of chronic shortage of donors, many patients are currently anticipating corneal transplantation in Japan. In addition, patients may experience rejection in the case of transplantation of a cornea from others. Corneal regenerative medicine is a new treatment method aiming to regenerate corneas, of which there is a chronic shortage, using the cutting-edge culturing and tissue engineering technologies and will enable transplantation therapy using our own cells.
Stevens-Johnson syndrome, ocular pemphigoid and thermochemical injury, which are caused by damage to the stem cells in the corneal epithelia, causes not only clouding of the cornea but also adhesion of the eyelids and dry eye. Therefore, it was impossible to cure them by corneal transplantation with donated cornea. This is why these disorders have been regarded as intractable keratoconjunctival disorders and considered to be incurable for years.
Kyoto Prefectural University of Medicine has been doing research on corneal epithelial regenerative medicine for years in patients with these intractable keratoconjunctival disorders. Based on the results, Kyoto Prefectural University of Medicine began to provide “cultivated autologous oral mucosal epithelial cell sheet transplantation” as an advanced medical care in January 2014
Target disease
Cultivated autologous oral mucosal epithelial cell sheet transplantation is mainly performed for the treatment of intractable keratoconjunctival disorders, namely Stevens-Johnson syndrome, thermochemical injury and ocular pemphigoid, which are caused by damage to the stem cells in the corneal epithelia.
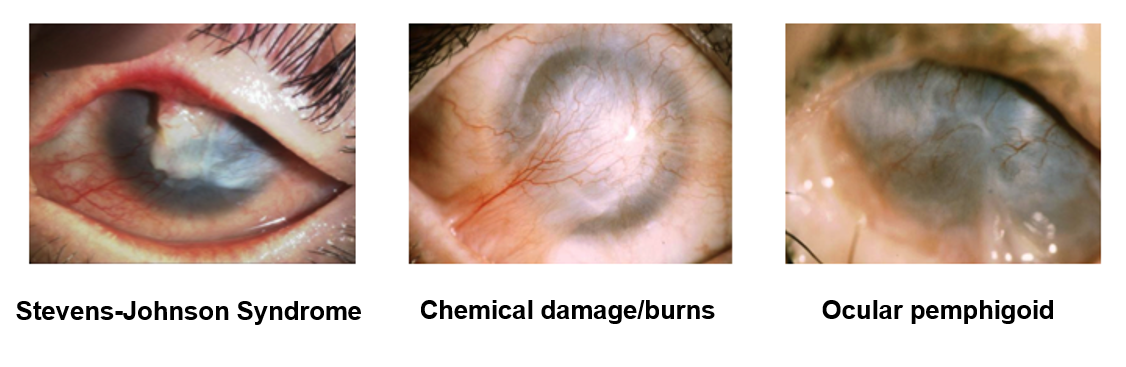
Stevens-Johnson syndrome develops as drug eruption in most cases and causes a sudden high fever, rash and erosion on the skin mucosa and severe inflammation on the surface of the eye, including the cornea. Even after recovery of the general condition, sticking of the eyelid and the cornea (“adhesion”) and corneal epithelial defect (wound in the iris) will not resolve and will continuously be aggravated, resulting in difficulty seeing or almost no eyesight because of clouding of the cornea (iris).
Thermochemical injury is a collective for burns and chemical damage (damage by chemicals) and occurs in an accident during an experiment or construction. The surface of the eye will become inflamed, and it will be impossible to repair it. Even after recovery, thermochemical injury will result in difficulty seeing or almost no eyesight because of sticking of the eyelid and the cornea (iris) (“adhesion”) and clouding of the cornea (iris) just as Stevens-Johnson syndrome.
Ocular pemphigoid is an autoimmune disease (a disease due to abnormalities in the immune system) that develops in the elderly and causes adhesion on the surface of the eye that often progresses slowly. Corneal epithelial defect (wound in the iris) suddenly develops and is sometimes aggravated without being cured. In both cases, aggravation will result in difficulty seeing or almost no eyesight because of clouding of the cornea (iris).
These disorders have been difficult to be cured with the conventional corneal transplantation using a donated cornea, which temporarily achieves good visual acuity but results in visual acuity equivalent or worse than that before surgery in most cases in the long run. However, the disorders can currently be treated because of technical development of corneal regenerative medicine.
When is the treatment performed?
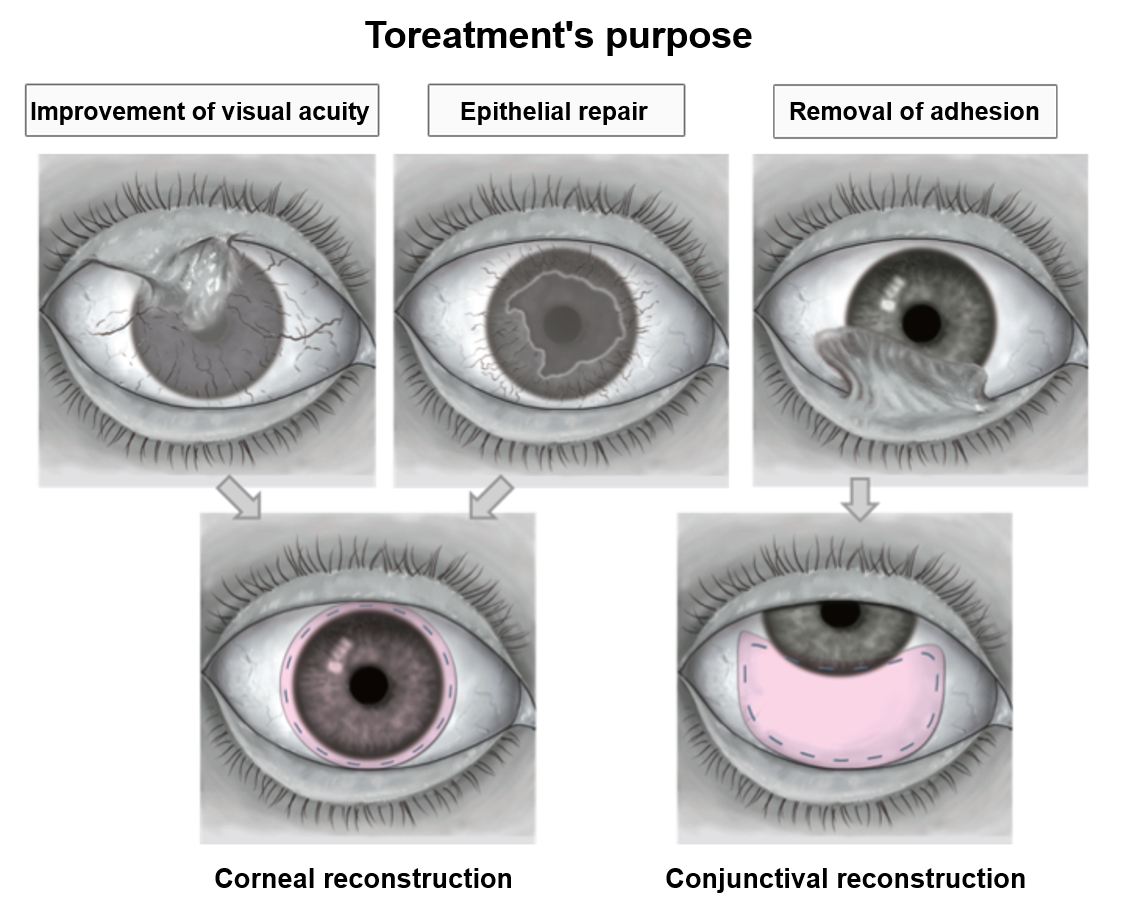
Intractable keratoconjunctival disorders involve corneal opacity (clouding of the iris) accompanied by adhesion. Adhesion and opacity are caused by abnormal mucosa on the surface of the eye. By removing the abnormal mucosa and transplanting a clean epithelial sheet, visual acuity will be improved (corneal reconstruction for the purpose of improving visual acuity).
As described above, these disorders may cause corneal epithelial defect (wound in the iris), which may be aggravated to vision loss without being resolved. For the treatment of such incurable epithelial defect, a clean epithelial sheet will be transplanted to avoid vision loss (corneal reconstruction for the purpose of epithelial repair).
Among intractable keratoconjunctival disorders, adhesion of the conjunctiva (white part of the eye) will be gradually aggravated with ocular pemphigoid. Because of the inability to close your eye(s), the condition of the cornea (iris of the eye) will be aggravated and result in decreased visual acuity. You can prevent aggravation of the disease by removing the adhesion and transplanting the epithelial sheet before you experience decreased visual acuity (conjunctival reconstruction for the purpose of removal of adhesion).
In addition, when surgery is performed for the treatment of cataract advanced because of intractable keratoconjunctival disorders, adhesion will often be aggravated after surgery and result in visual acuity that is worse than that before surgery. By transplanting an epithelial sheet on the area where adhesion has been removed, cataract surgery can be performed safely, which will lead to prevention of postoperative aggravation (conjunctival reconstruction for the purpose of removal of adhesion).
Regenerative medicine for the cornea provided by Kyoto Prefectural University of Medicine
Kyoto Prefectural University of Medicine is aiming to develop a new treatment method to maintain and recover the visual function by producing an epithelial sheet from the oral mucosal cells of the patient and transplanting it to promote regeneration of the tissues.
First, epithelial cells will be isolated from the patient’s oral mucosal cells. These epithelial cells will be dispersedly spread on a donated amniotic membrane and cultivated along with the cells used subsidiarily to create an environment necessary for proliferation and differentiation (feeder cells) for about two weeks at the Cell Processing Center (CPC). An epithelial sheet will be produced in this way, and the quality and safety of the sheet will be confirmed before transplantation.
The sheet prepared in this way will be transplanted on the cornea using instruments equivalent to those used for common corneal transplantation. For six months after surgery, tests such as visual acuity test, funduscopy and diagnostic imaging will be performed according to the study protocol to confirm safety and evaluate efficacy.
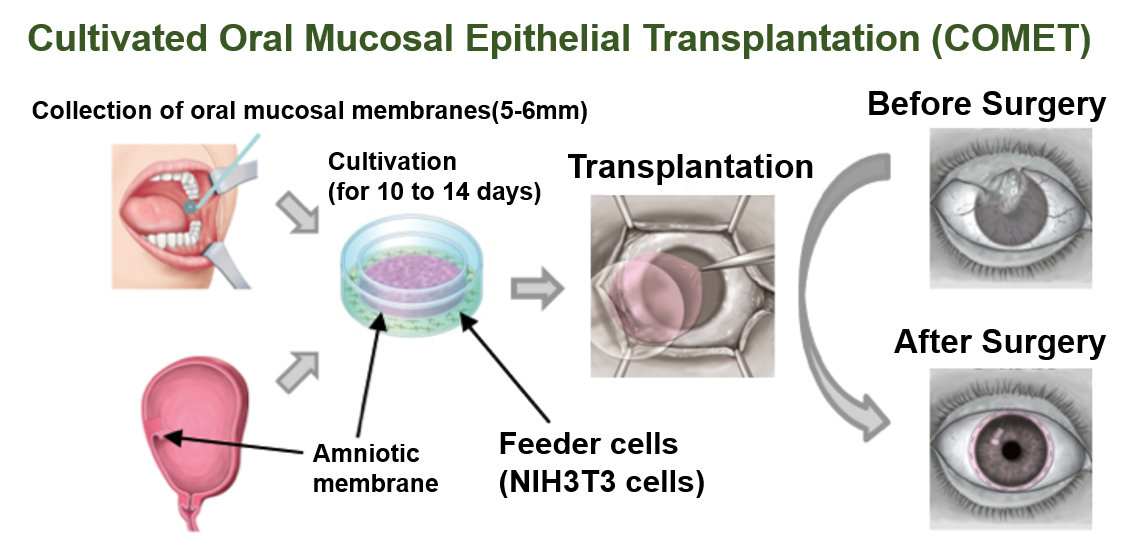
This sheet transplantation is performed at Kyoto Prefectural University of Medicine. This sheet is manufactured at the Cell Processing Center (CPC) at the Foundation for Biomedical Research and Innovation at Kobe. At Kyoto Prefectural University of Medicine, this treatment has been performed in 106 eyes in 93 patients since 2002. Among them, detailed analyses were performed in 81 eyes in 72 patients who had undergone the surgery by December 2008, and efficacy has been confirmed.
Major test items and monitoring parameters and the schedule of the tests/monitoring at Kyoto Prefectural University of Medicine
Hospitalization is supposed to last 1 to 3 weeks, and prescribed tests will be performed on the postoperative Day 2 and Weeks 1, 4, 12 and 24 (See “○” in the table).
Monitoring parameters/test items/endpoints
| Test timing /Test item |
Before Transplantation | After Transplantation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B e f o r e e n r o l l m e n t * 1 |
S e l e c t i n g O r a l M u c o s a |
O n t h e d a y o f t r a n s p l a n t a t i o n |
2 d a y s * 2 |
1 W e e k * 2 |
2 W e e k s * 2 |
4 W e e k s * 2 |
8 W e e k s * 3 * 4 |
12 W e e k s * 3 |
16 W e e k s * 3 * 4 |
20 W e e k s * 3 * 4 |
24 W e e k s * 3 |
|
| Subject background factors | 〇 | |||||||||||
| Clinical laboratory tests *5 | 〇 | 〇 | 〇 | 〇 | ||||||||
| Basic Examination A | 〇 | 〇 | △ | 〇 | △ | 〇 | △ | △ | 〇 | |||
| Basic Examination B | 〇 | 〇 | 〇 | 〇 | 〇 | |||||||
| Ocular manifestation A | 〇 | 〇 | 〇 | △ | 〇 | △ | 〇 | △ | △ | 〇 | ||
| Ocular manifestation B | 〇 | 〇 | ||||||||||
| Ocular manifestation C | 〇 | △ | △ | △ | 〇 | |||||||
| Symptoms *6 | 〇 | 〇 | 〇 | 〇 | 〇 | |||||||
| Anterior eye photography | △ | △ | △ | △ | △ | △ | △ | △ | △ | △ | ||
| Usage of drugs | △ | △ | △ | 〇 | 〇 | △ | 〇 | △ | 〇 | △ | △ | 〇 |
| Usage of soft contact lens | 〇 | 〇 | 〇 | △ | 〇 | △ | 〇 | △ | △ | 〇 | ||
| Infection test | △ | |||||||||||
| Findings at transplantation | 〇 | |||||||||||
| Timing for case reporting | ● | ● | ● | ● | ● | |||||||
| Adverse Events | → | → | → | → | → | → | → | → | → | → | → | |
*1:Data collected within four weeks before enrollment can be used
*2:To be performed after transplantation, Day 2 (with an acceptable visit window between Day 1 and Day 3), Day 7 (with an acceptable visit window between Day 5 and Day 9) and Day 14 (with an acceptable visit window between Day 12 and Day 16).
*3:The acceptable visit windows will be ±7 days for Weeks 4, 8, 12, 16 and 20 and ±14 days for Week 24.
*4:The results of the tests scheduled for Weeks 8, 16 and 20 can be confirmed with a cooperating local doctor if the patient cannot visit Kyoto Prefectural University of Medicine because of a long trip to the hospital.
*5:The clinical laboratory tests scheduled for Week 12 (±7 days) and Week 24 (±14 days) will be performed only in subjects continuously under systemic medication.
*6:VFQ-25 will be used to check for symptoms.
Explanatory notes
○:Items necessary for a case report
△:Items not necessary for a case report
●:Timing for case reporting
To patients who hope to receive corneal regenerative treatment
At Kyoto Prefectural University of Medicine, the most appropriate method of corneal regeneration is selected according to the eye conditions in each patient. This treatment may not be applicable even if you wish to receive it.
Furthermore, the cultivated autologous oral mucosal epithelial cell sheet transplantation is not covered by health insurance. So, you have to cover your copayment for the use of Advanced Medical Care. If you wish to receive corneal regenerative treatment at Kyoto Prefectural University of Medicine, please send us a referral form from your primary-care doctor and visit the special outpatient clinic of our hospital (only on Mondays).