Distinctive Ocular Manifestations
The incidence of ocular complications associated with SJS/TEN is considered to be approximately 60%, and ocular clinical presentations (hyperemia and/or eye pain) often precede skin eruption. Therefore, when a patient already has bilateral hyperemia at the onset of skin eruption, he/she is likely to have ocular complications.
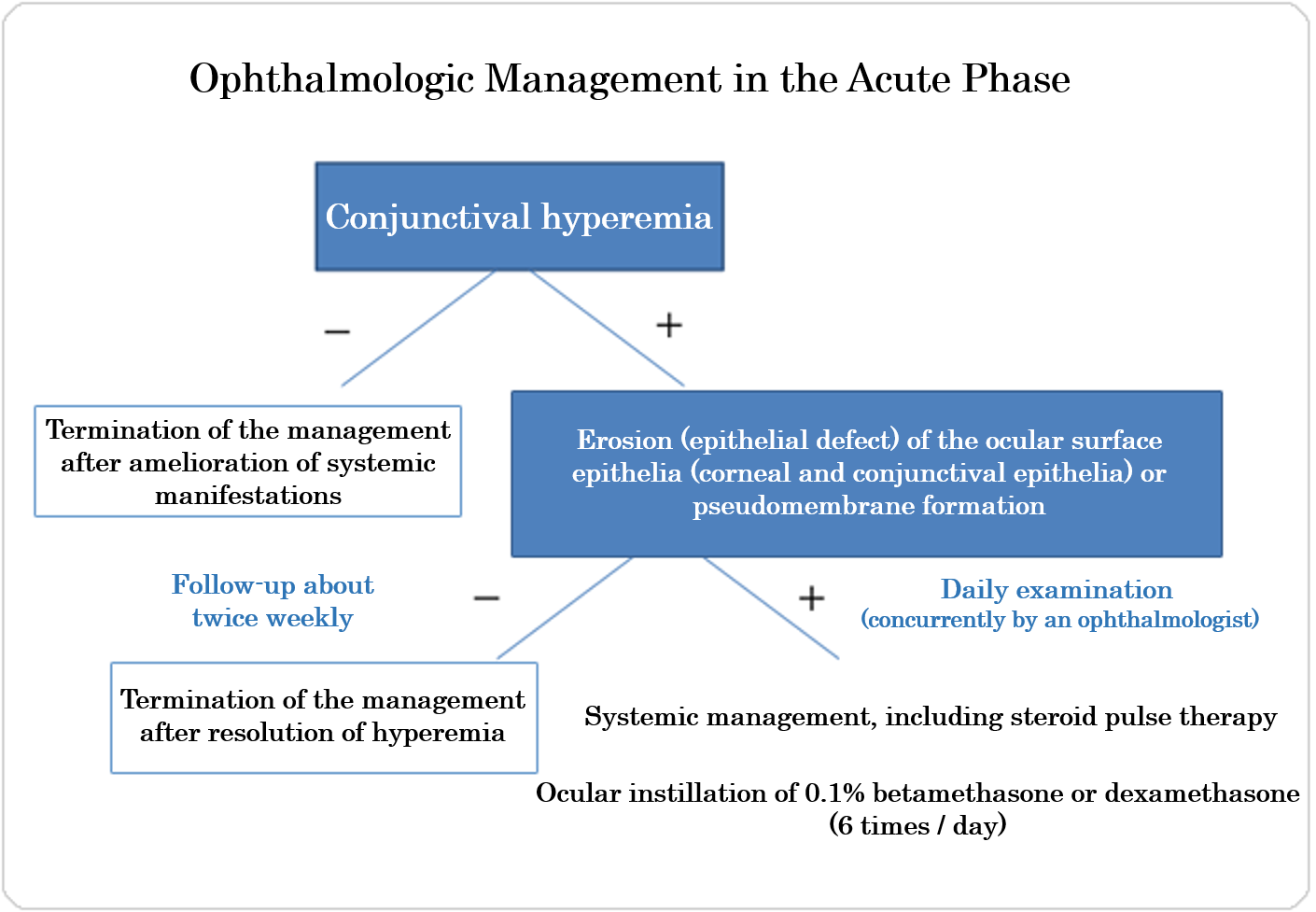
When a patient has any ocular clinical presentations in spite of mild skin eruption, he/she needs to visit an ophthalmologist as soon as possible (within 1 to 2 days) to have the ophthalmologic severity checked. When erosion of the ocular surface epithelia (epithelial defect) or pseudomembrane formation is detected, there is a high risk of ocular sequelae. Therefore, it is important to check the ocular manifestations from the early phase after onset and suppress inflammation on the ocular surface.
According to a survey by the Department of Ophthalmology, Kyoto Prefectural University of Medicine, all the patients with eye disorders had conjunctival hyperemia, oral and lip redness/erosion and paronychia. Bilateral hyperemia, perioral hemorrhage/erosion and redness at the bases of the nails are highly suggestive of serious ocular complications.

Distinctive Ocular Manifestations in the Acute Phase
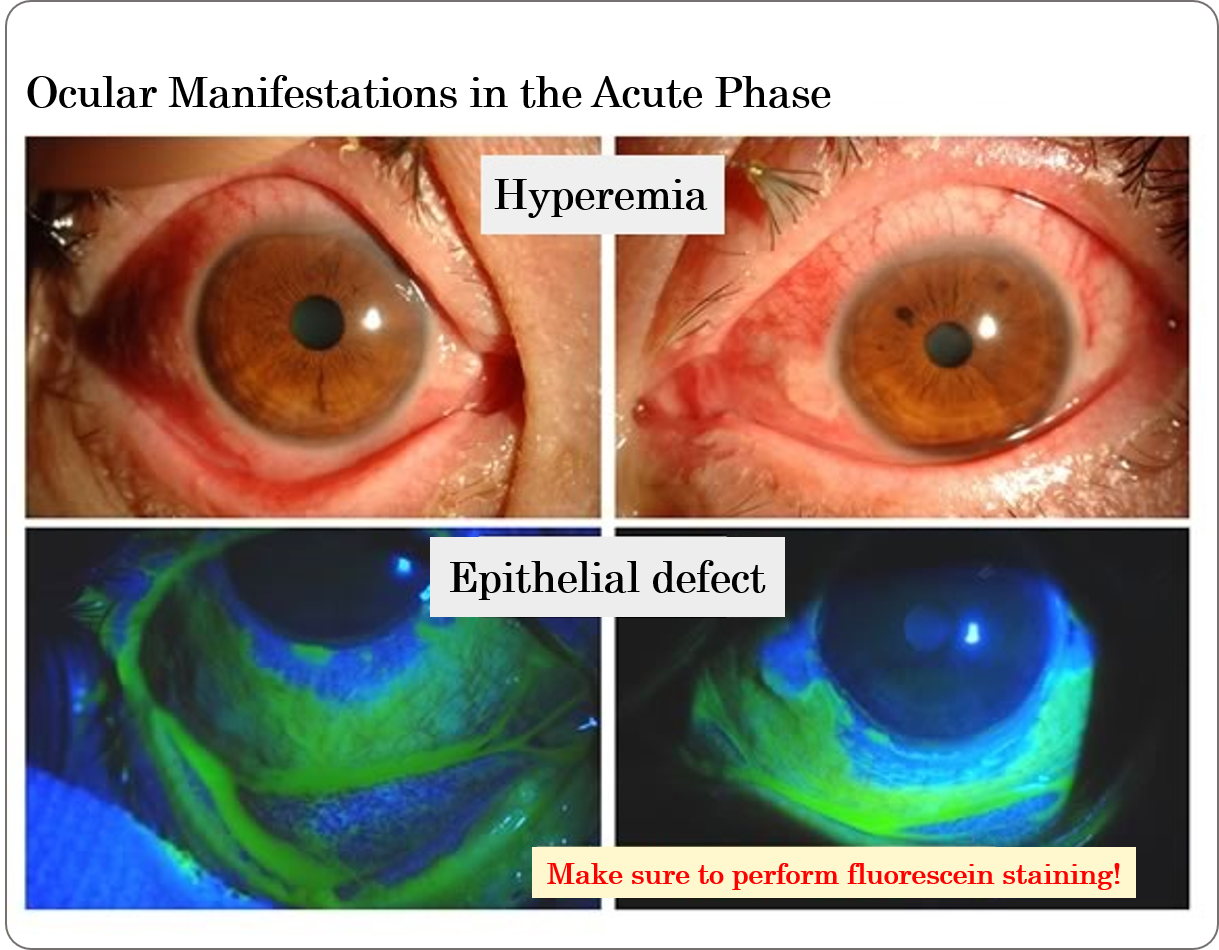
Hyperemia
Conjunctival hyperemia will be noted in both eyes. Even when hyperemia looks mild, extensive epithelial defect may be present concomitantly. Therefore, macroscopic evaluations involve a risk (See the figure below). Careful attention should be paid to patients who cannot open their eyes because of pain. When a patient is suspected of having ocular complications (hyperemia and eye pain), he/she should be referred to an ophthalmologist to have presence of “erosion of the ocular surface epithelia (epithelial defect)” or “pseudomembrane” checked.
Erosion (epithelial defect) of the ocular surface epithelia (corneal and conjunctival epithelia)
Punctate epithelial disorder, corneal or conjunctival epithelial defect and extensive keratoconjunctival epithelial defect will develop on the ocular surface epithelia (corneal and conjunctival epithelia) respectively in mild cases, moderate cases and severe cases. When a patient has punctate epithelial disorder, he/she may experience epithelial defect in a few days.
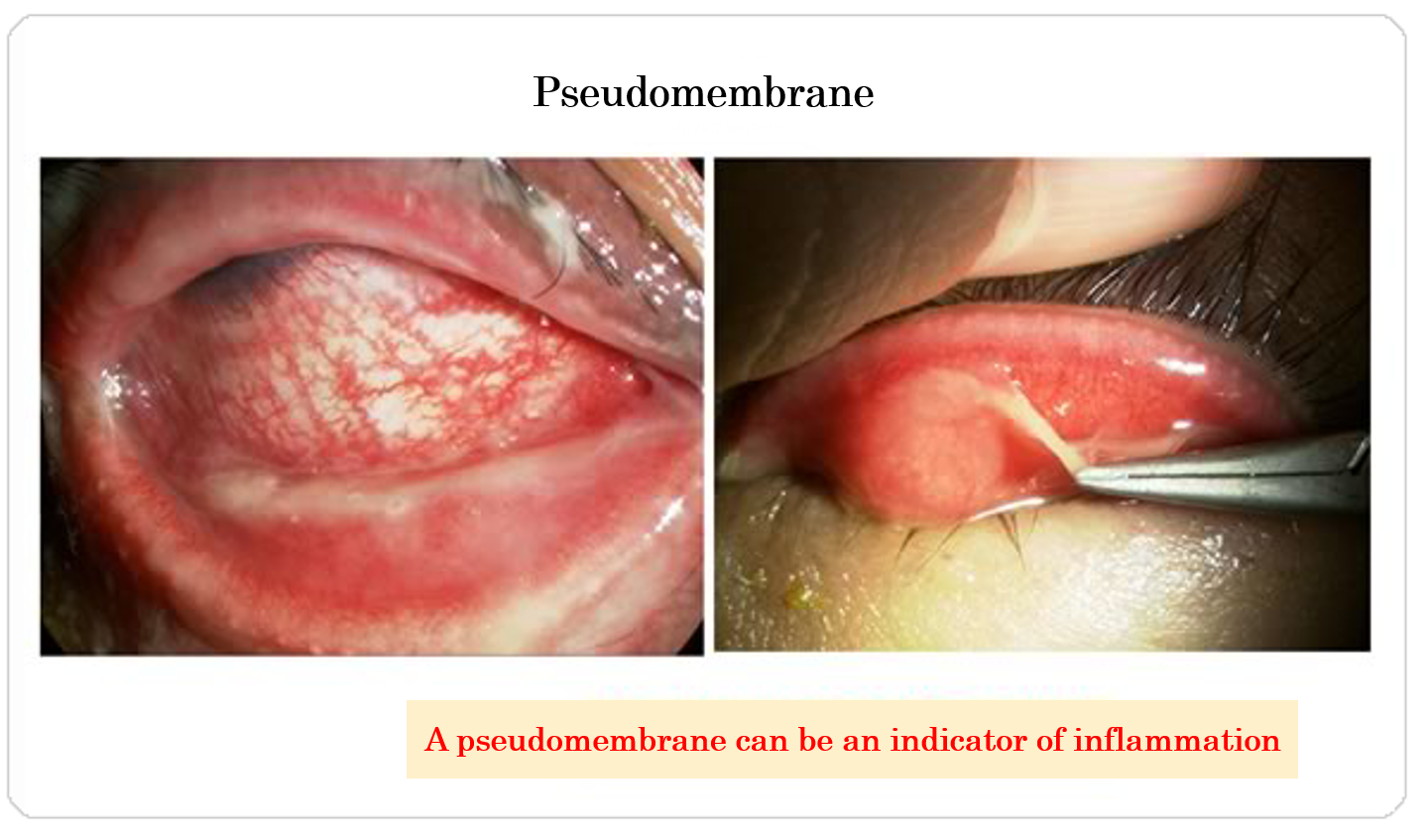
Pseudomembrane Formation
A pseudomembrane, which is composed of fibrin, necrotized epithelial cells and infiltrating cells (mainly neutrophils), indicates severe inflammation on the ocular surface. If treatment works, pseudomembrane will spontaneously become milder. Increased pseudomembrane formation noted during treatment suggests aggravation of inflammation on the surface of the eye.
Symblepharon
Severe inflammation will develop also in the eyelids and will be accompanied by redness/swelling of the eyelids. It will also be accompanied by “loss of eyelashes” in severe cases. Symblepharon (adhesion of the eyelid and the eyeball) will rapidly progress with inadequate suppression of inflammation or severe inflammation.
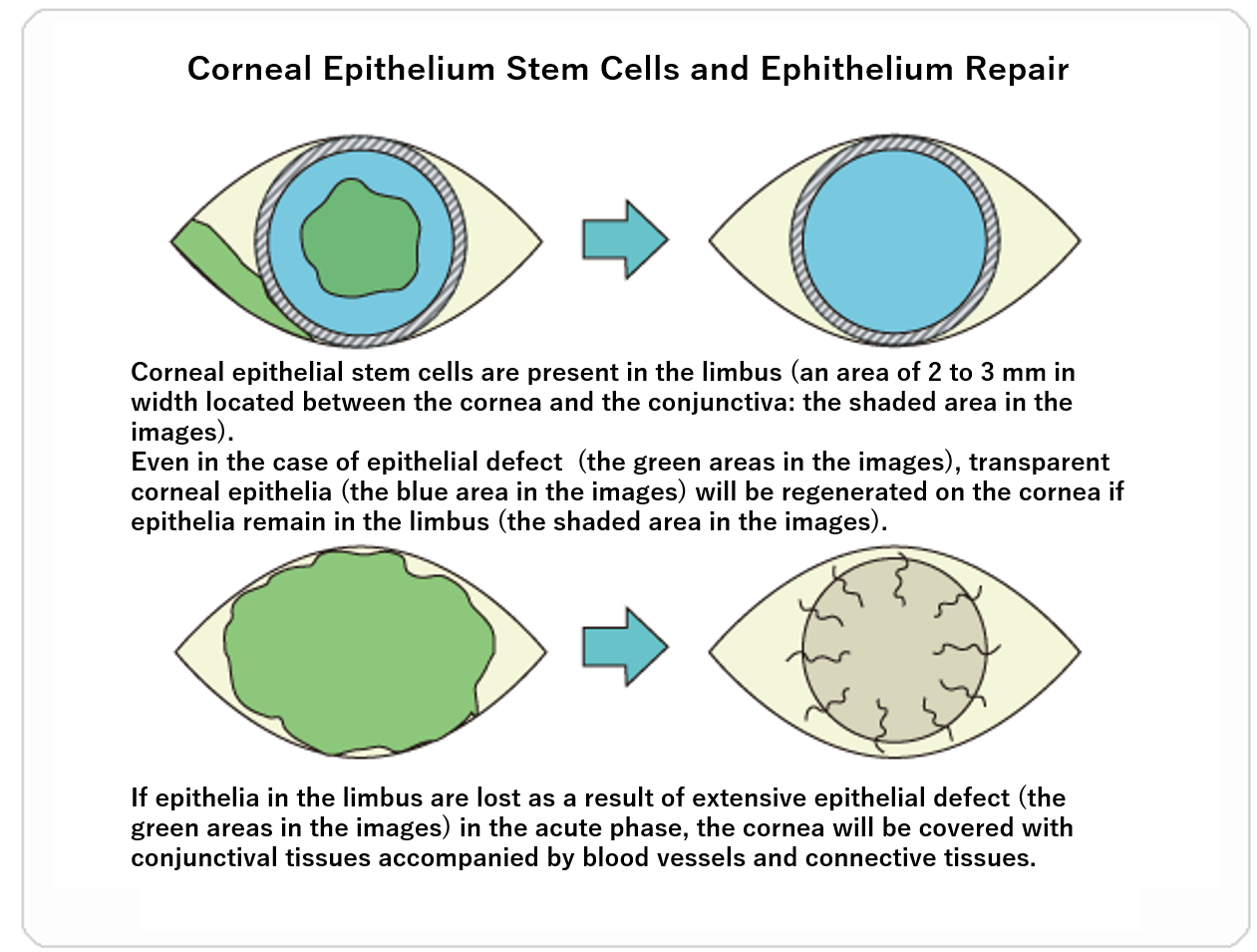
Clinical Condition
Corneal epithelial stem cells are present in the area called the limbus, which is 2 to 3 mm wide and located between the cornea and conjunctiva. In the acute phase of SJS/TEN, when skin eruption and erosion are noted on the skin and mucous membranes throughout the body, inflammation will develop on the ocular surface and cause erosion (epithelial defect). The consequent loss of all the epithelia in the limbus will make it impossible for the limbus to supply corneal epithelia, and conjunctival epithelia will subsequently expand over the cornea. Along with the conjunctival epithelia, blood vessels will invade the cornea, which is normally transparent, and opacify it. Even in the case of corneal epithelial erosion (epithelial defect), the cornea will be repaired by corneal epithelia to maintain its transparency if epithelia remain in the limbus (See the figure below).
Distinctive Ocular Manifestations in the Chronic Phase
The main clinical presentations noted in the chronic phase are visual impairment and dry eye, which are followed by uncomfortable clinical presentations of trichiasis and cicatricial changes such as symblepharon. Patients need to pay routine visits to an ophthalmologist for ocular surface management.
Dry eye
Lacrimal fluid is composed of mucus and an oily component as well as water. Patients with SJS have dry eye with a lack of all of them, which is considered to be caused by loss of goblet cells and the meibomian glands respectively secreting mucus and oil into tears, as well as lacrimal ductal obstruction. Even with replacement of artificial tears, the surface of the eye will get dry because of rapid evaporation, which will cause the clinical presentations such as eye pain, feeling of dryness and difficulty opening the eyes.
Corneal opacity
If the conjunctival epithelia, together with blood vessels and connective tissues, cover the surface of the cornea, the corneal surface will become opaque and unlevel and cause visual impairment. The regenerated epithelia will be abnormally differentiated, and the ocular surface will become keratinized like the skin.
Trichiasis
Trichiasis is noted as a sequela of inflammation.
Symblepharon
Adhesion develops in association with repair of the epithelial defect in the acute phase.
Chronic Conjunctivitis
The condition of the ocular surface will be stabilized, but non-specific inflammation will be still present in the chronic phase. In some patients, the lesion will be aggravated with repeated mild relapse.
Grading of the Ocular Manifestations in the Chronic Phase of SJS/TEN
A grading system has been established for the following 13 items for evaluation of scarring of the ocular surface in order to reveal distinctive ocular manifestations in the chronic phase of SJS/TEN.
Corneal manifestations
Limbus stem-cell deficiency, invasion of conjunctiva, invasion of blood vessels, corneal opacity, keratinization, epithelial defect, superficial punctate keratopathy
Conjunctival manifestationss
Hyperemia, Symblepharon
Eyelid manifestations
Trichiasis, Mucosal Membrane Transition Region, Meibomian Gland Opening, Lacrimal Point Closure
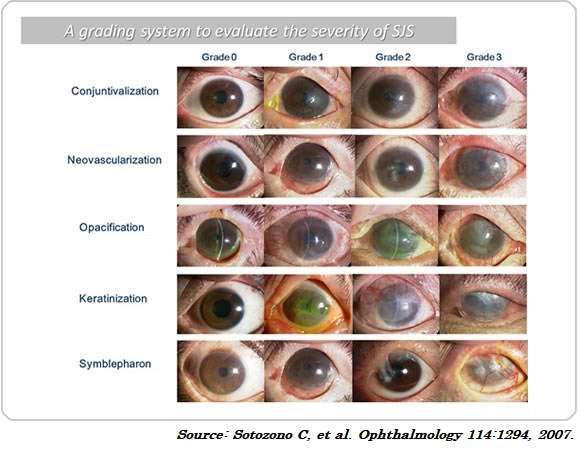
In an analysis performed in 138 eyes in patients with SJS visiting an ophthalmologist, complete loss of the epithelia in the limbus was noted in ≥80% of the analyzed eyes, and neovascularization, opacification and symblepharon were frequently noted (See the figure below).
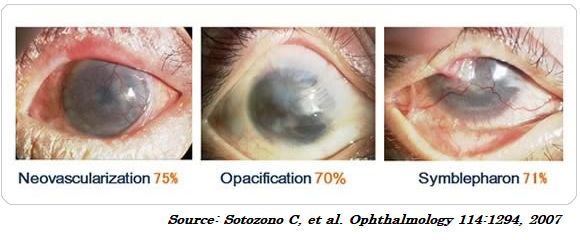
This clinical scoring is highly appreciated internationally and has been used in order to evaluate patients applicable to cultivated oral mucosal epithelial cell sheet transplantation or limbal-supported contact lenses and the postoperative findings from the patients.